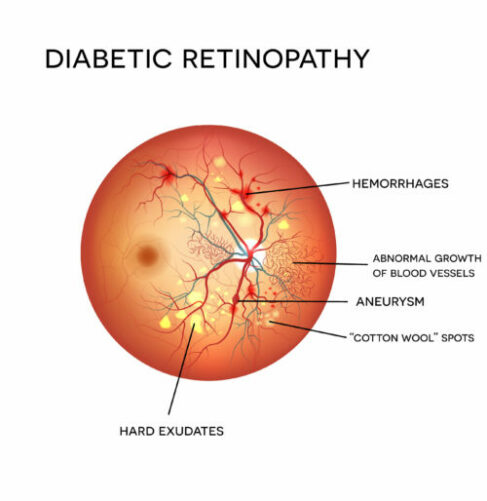
Diabetes is a condition in which the body’s ability to process and store sugar has been impaired. Among the characteristics of the disease are gradual changes in blood vessels. Diabetic retinopathy is a complication of diabetes caused by the deterioration of blood vessels nourishing the retina in the back of the eye. As the blood vessels weaken, they may leak fluid or blood into the clear vitreous mass that fills the eye or becomes enlarged, damaging the delicate retina.
Who Is At Risk?
Persons who have had diabetes for a number of years are especially at risk of developing diabetic retinopathy. Six in ten who have had diabetes for over 15 years show symptoms of retinal damage; high blood pressure and pregnancy both worsen the condition. Although diabetic retinopathy is easily detected during routine eye examinations and treatable with laser surgery in the early stages, it is the leading cause of new blindness among adults. Diabetics are 25 times more likely to become blind than those without the disease.
Two Stages of Retinopathy
In Non-Proliferative Diabetic Retinopathy, blood vessels weaken and begin to leak blood and serum. These fluids collect and form deposits in the retinal tissues, causing it to swell. If the leaking blood vessels are in the peripheral area of the eye, no serious visual impairment usually occurs. However, if the fluid collects in the macula it can cause blind spots and blurred vision which make activities such as reading and driving difficult or impossible.
In the second and more advanced stages of proliferative diabetic retinopathy, the abnormal cells rapidly spread across the inner surface of the retina. These weakened vessels can bleed into the vitreous and stop light from reaching the retina. In addition, the connective scar tissue, which forms as a result of the ruptured blood vessels, can shrink, pulling the retina away from its underlying structure, causing it to detach. Severe loss of sight – even blindness – may result.
There is no pain associated with either form of retinopathy. A gradual blurring of vision may occur, but changes in the eye can go undetected without a medical eye exam. When bleeding occurs in proliferative retinopathy, the patient may see spots, a clouding of vision, or experience a complete loss of sight in the affected eye.
Detection and Diagnosis
Examination under a microscope/slit-lamp allows your doctor to view your retina and other structures of the eye. The Cirrus HD-OCT is the first spectral domain technology instrument to offer high definition 3D maps of individual retinal layers to reveal pathology hidden within the retinal tissue.
Some patients are given an intravenous injection of fluorescein dye in a procedure called fluorescein angiography. The dye, which takes only moments to reach the eye, makes tiny blood vessels visible, enabling photographs to be taken for careful study. At the Omaha Eye & Laser Institute and Lincoln Eye & Laser Institute, we offer the latest digital imaging to allow immediate analysis of your fluorescein angiography. This will help us explain to you and your family any problems with the retina and how to best treat you.
Retinopathy
Dr. William Thomas will take into account your age, medical history, lifestyle, and the degree of damage to the retina before recommending a course of action. In many cases, treatment is not required; in others, laser treatments may be recommended to halt further progression of the disease.
In cases of diabetic macular edema (DME), Dr. Thomas treats with intravitreal injections, to include Avastin, Eylea and Lucentis. These anti-vegf treatments are injected into the vitreous cavity in a sterile fashion. This injection will not cure the disease; however, in most cases, it will improve vision. Monthly visits are recommended to determine further course of treatment. If left untreated DME could cause substantial vision loss.
If the vitreous has become too clouded with blood to clear on its own, Dr. Thomas may proceed with a procedure called a vitrectomy with laser photocoagulation. In this technique, the vitreous is drained and replaced with air or solution. An immediate improvement in sight is noted in about 70% of cases.
What is a Macular Pucker?
A macular pucker is an extra layer of tissue that has formed on the eye’s macula. The macula is located in the center of the retina, an area of light-sensitive cells at the back of the eye. The macula is responsible for central vision, which is the sharp, straight-ahead vision we need for reading, driving, and seeing fine detail.
A macular pucker can cause blurred and distorted central vision. It is usually related to aging and happens in people over age 50.
What are the symptoms of a macular pucker?
The main symptom of macular pucker is a change in vision. Vision changes and loss can range from none to severe, but severe vision loss is uncommon. People with a macular pucker might notice that their vision is blurry or slightly distorted, and straight lines can appear wavy. They might have difficulty seeing fine details and reading the small print. They might also have a gray area in the center of vision or even a blind spot.
How is a macular pucker treated?
A macular pucker usually does not need treatment. Some puckers may resolve on their own. In serious cases, people with macular pucker develop vision problems that are severe enough to interfere with their daily activities. These people might need surgery to treat their macular pucker. This surgery is called vitrectomy with membrane peel.
What is a Macular Hole?
A macular hole is a small break in the macula, located in the center of the eye’s light-sensitive tissue called the retina. A macular hole can cause blurred and distorted central vision. Macular holes are related to aging and usually occur in people over age 60.
What are the symptoms of a macular hole?
Macular holes often begin gradually. In the early stage of a macular hole, people may notice a slight distortion or blurriness in their straight-ahead vision. Straight lines or objects can begin to look bent or wavy. Reading and performing other routine tasks with the affected eye become difficult.
Is a macular hole the same as age-related macular degeneration?
No. Macular holes and age-related macular degeneration are two separate and distinct conditions, although the symptoms for each are similar. Both conditions are common in people 60 and over. An eye care professional will know the difference.
Is my other eye at risk?
If a macular hole exists in one eye, there is a 10-15 % chance that a macular hole will develop in your other eye over your lifetime. Your doctor can discuss this with you.





