The cornea plays a crucial role in focusing light and maintaining sharp vision. When corneal damage or disease starts affecting your eyesight, a corneal transplant may become necessary to restore functional vision.
Keep reading to learn more about which conditions may require this specialized surgery so you can make informed decisions about your eye care.
What is the Cornea?
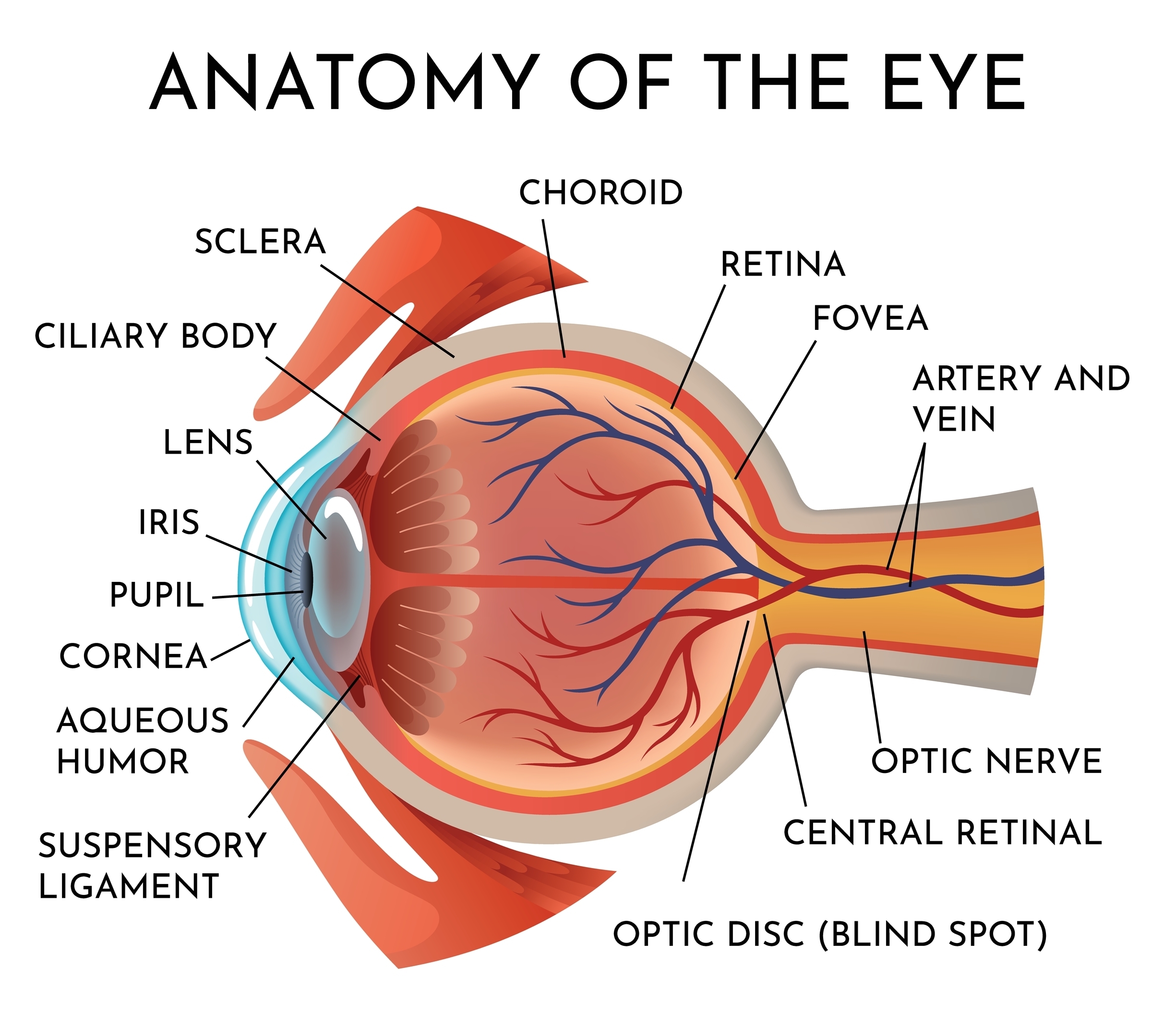
Your cornea is the transparent tissue covering the front of your eye, protecting the iris and pupil while providing approximately two-thirds of your eye’s focusing power. It consists of five distinct layers that work together to maintain clarity and proper light refraction.
The cornea’s innermost layer, called the endothelium, contains a finite number of cells that maintain corneal clarity and do not regenerate. When these cells become damaged or diseased, vision problems often result, sometimes requiring surgical intervention.
Primary Conditions Requiring Corneal Transplantation
While being diagnosed with a corneal condition does not automatically mean you will need a corneal transplant, severe cases of these conditions that don’t respond to less invasive treatments may require transplantation:
Keratoconus
Keratoconus is one of the most common reasons for corneal transplantation in younger patients. This progressive condition causes the cornea to gradually thin and bulge into a cone-like shape, creating irregular astigmatism that cannot be adequately corrected with glasses or standard contact lenses.
The disease typically develops during puberty, and while the direct cause is unknown, keratoconus may be linked to genetics and excessive eye rubbing. Specialty contact lenses can manage many cases, but patients with advanced keratoconus who cannot achieve functional vision with contact lenses often require corneal transplantation.
The Omaha and Lincoln Eye and Laser Institute offers corneal crosslinking treatment, a less invasive procedure that can help stabilize the cornea and potentially prevent the need for transplantation in some candidates.
Fuchs’ Endothelial Dystrophy
This hereditary condition affects the innermost layer of the cornea, causing cells to deteriorate and allowing fluid to accumulate within the corneal tissue. Patients with Fuchs’ dystrophy typically experience cloudy, hazy vision that worsens throughout the day as corneal swelling increases.
Early stages can often be managed with specialized eye drops that help dehydrate the cornea. However, when vision cannot be adequately restored with medical treatment, a partial-thickness corneal transplant called DSAEK (Descemet’s Stripping Automated Endothelial Keratoplasty) may be recommended.
Other Corneal Dystrophies
Various inherited corneal dystrophies can affect different layers of the cornea, potentially requiring transplantation when vision becomes significantly impaired. These conditions typically develop gradually and may affect both eyes, though often asymmetrically.
Corneal Scarring
Severe corneal scarring can result from various causes, including chemical burns, blunt trauma, viral infections, or bacterial infections. When scarring significantly impairs vision and cannot be improved through other treatments, corneal transplantation may be necessary.
The type of transplant depends on which corneal layers are affected. Surface scarring might require only a partial-thickness transplant, while deeper scarring affecting multiple layers may necessitate a full-thickness replacement.
Previous Surgical Complications
Sometimes complications from previous eye surgeries can damage the cornea sufficiently to require transplantation. This might occur after cataract surgery, glaucoma procedures, or previous corneal surgeries that resulted in corneal decompensation or scarring.
When Is Corneal Transplant Surgery Recommended?
Your ophthalmologist will consider several factors when determining whether corneal transplantation is appropriate:
Visual Function

The most important consideration is whether your current vision prevents you from performing necessary daily activities or work responsibilities. Visual acuity needs vary among individuals, as some patients may require 20/20 vision for their profession, while others function well with 20/60 vision.
Contact Lens Tolerance
Before recommending transplantation, especially for keratoconus, your eye care team will ensure that specialty contact lens options have been thoroughly explored. Many patients initially referred for transplant can achieve functional vision with properly fitted specialty lenses.
Progressive Disease
For conditions like keratoconus with progressive thinning, significant decentering, or blood vessel growth into the cornea, earlier transplantation may be recommended to prevent complications and ensure optimal surgical outcomes.
Pain or Recurrent Infections
When corneal disease causes persistent pain or frequent infections that cannot be controlled with medical treatment, transplantation may be necessary for comfort and eye health.
What to Expect During Your Evaluation
The team at The Omaha and Lincoln Eye and Laser Institute conducts comprehensive evaluations to determine the most appropriate treatment approach. This assessment includes detailed corneal mapping, measurement of corneal thickness, evaluation of endothelial cell health, and careful consideration of your visual needs and lifestyle requirements.
Your ophthalmologist will discuss all available options, including medical treatments, specialty contact lenses, and surgical interventions. The goal is to achieve the best possible vision while minimizing risks and recovery time.
What Will My Vision Be Like After Corneal Transplantation?

Corneal transplant success rates are generally high, with most patients achieving significantly improved vision. However, recovery varies depending on the type of transplant performed.
Partial-thickness procedures typically offer faster visual recovery, while full-thickness transplants require more extensive healing time. Regular follow-up care is essential for monitoring transplant health and detecting any signs of rejection early.
With proper care and monitoring, corneal transplants can provide clear vision for many years to come. If you’re experiencing vision problems that may be related to corneal disease, schedule a comprehensive evaluation to discuss your treatment options.
Early intervention can often preserve vision and reduce the need for more extensive surgical procedures. Contact The Omaha and Lincoln Eye and Laser Institute in Omaha or Lincoln, NE, today to learn more about corneal transplant options and determine the best approach for preserving and restoring your vision.





